Introduction: Unlocking the Power of Interoperability in Australian Healthcare
Interoperability is the backbone of a connected, efficient, and patient-centric healthcare system. In a world increasingly driven by data, the ability for healthcare systems to seamlessly exchange information is no longer a luxury—it’s a necessity. At the heart of this transformation lies FHIR (Fast Healthcare Interoperability Resources), a standard designed to improve how data flows across healthcare systems, ensuring patients receive better, safer, and more efficient care.
Australia’s healthcare sector has been steadily progressing toward the adoption of FHIR. Government initiatives, private sector involvement, and technological advancements are collectively shaping a future where interoperability is achievable and beneficial to all stakeholders, from patients to providers.
However, this transition is not without challenges. FHIR adoption requires not only technical readiness but also organizational willingness and strategic alignment. The Australian government, industry leaders like CSIRO, and technology providers such as Microsoft Azure are leading the charge, creating frameworks and solutions to accelerate adoption. Organizations like Blue Owls Solutions further ease the path by offering managed services tailored to healthcare providers’ unique needs.
In this blog, we delve into:
- The current state of FHIR adoption in Australia,
- CSIRO’s groundbreaking Sparked Initiative,
- The release of the AU Core FHIR Implementation Guide,
- The imperative for healthcare organizations to become technology-ready,
- The transformative potential of Azure Health Data Services’ FHIR Service,
- How Blue Owls Solutions supports organizations through a managed service approach.
Let’s explore these topics in detail, beginning with the current Australian context for FHIR adoption.
1. Current Australian Context on Adoption of FHIR
Australia has long been at the forefront of healthcare innovation, and the adoption of FHIR is a testament to this commitment. As a globally recognized standard for exchanging healthcare information electronically, FHIR supports the interoperability of electronic health records (EHRs), enabling diverse systems to “speak the same language.”
Key Drivers for FHIR Adoption in Australia
Australia’s healthcare ecosystem is uniquely positioned to benefit from FHIR due to several factors:
- Government Mandates: The Australian Digital Health Agency (ADHA) has prioritized interoperability, emphasizing the importance of FHIR in its National Digital Health Strategy. Initiatives like My Health Record rely on FHIR to ensure consistent data exchange.
- Patient-Centric Care: With increasing demand for patient empowerment, FHIR facilitates real-time access to health data, empowering individuals to take an active role in their care.
- Ecosystem Collaboration: Australia’s healthcare system involves diverse stakeholders, including hospitals, private clinics, and community services. FHIR provides the common language needed for seamless data exchange across these entities.
Challenges in FHIR Implementation
While FHIR offers immense potential, its adoption in Australia faces hurdles such as:
- Fragmented Systems: Many legacy systems lack interoperability capabilities, requiring significant upgrades or replacements.
- Skill Gaps: Expertise in implementing and managing FHIR-based systems is still developing, necessitating workforce training.
- Compliance Complexity: Adhering to both local and global standards can be challenging, especially for smaller providers.
Real-World Examples of FHIR in Action
Despite these challenges, several projects demonstrate the progress being made:
- My Health Record: This national initiative uses FHIR to ensure healthcare providers and patients can access and share data securely.
- Hospital Integrations: Leading Australian hospitals, such as those in the Sydney Local Health District, have begun integrating FHIR-based solutions to improve patient data access and care coordination.
- Research Collaboration: CSIRO, through its work on the Sparked Initiative (explored in the next section), is pushing the boundaries of how FHIR can enable cutting-edge research and analytics.
As Australia continues its journey toward interoperability, initiatives like CSIRO’s Sparked Initiative play a pivotal role in addressing challenges and driving progress.
2. CSIRO’s Sparked Initiative
The Commonwealth Scientific and Industrial Research Organisation (CSIRO) has been instrumental in advancing healthcare innovation in Australia. Among its various initiatives, the Sparked Initiative stands out for its transformative impact on FHIR adoption and interoperability.
What Is the Sparked Initiative?
The Sparked Initiative, launched by CSIRO, is designed to accelerate the adoption of FHIR across Australia’s healthcare sector. By providing research-driven insights, technical tools, and collaboration frameworks, Sparked aims to bridge the gap between technology and real-world healthcare needs.
Objectives and Scope
- Promoting Standards: Educating stakeholders about FHIR’s potential and guiding its implementation.
- Developing Tools: Creating software and frameworks to simplify FHIR integration.
- Facilitating Research: Enabling healthcare data analytics and research through interoperable systems.
- Building Partnerships: Collaborating with healthcare providers, technology vendors, and policymakers.
Key Contributions to FHIR Adoption
- FHIR Ontoserver: A cornerstone of the Sparked Initiative, the Ontoserver simplifies terminology management and ensures consistent use of clinical terminologies across FHIR-based systems.
- Health Data Interoperability Pilot Projects: CSIRO has worked with healthcare providers to demonstrate the practical benefits of FHIR, from reducing administrative burdens to enhancing patient outcomes.
- Capacity Building: Training programs and workshops have been conducted to equip the healthcare workforce with FHIR knowledge and skills.
Impact on Interoperability
The Sparked Initiative has significantly boosted interoperability in Australia by:
- Reducing the time and cost associated with integrating disparate systems.
- Enhancing the quality of data exchanged between providers.
- Laying the foundation for advanced applications, such as predictive analytics and AI-driven decision support.
The Sparked Initiative exemplifies how research, collaboration, and technology can converge to solve complex challenges in healthcare. The next key milestone in Australia’s FHIR journey is the release of the AU Core FHIR Implementation Guide, which provides a standardized framework for adoption.
3. Release of AU Core FHIR Implementation Guide
The release of the AU Core FHIR Implementation Guide (AU Core FHIR IG) represents a landmark achievement in Australia’s interoperability journey. As a tailored version of the global FHIR standard, the AU Core FHIR IG provides specific guidance on how Australian healthcare providers and organizations can implement FHIR in a way that aligns with national priorities, regulatory requirements, and clinical needs.
Overview of the AU Core FHIR IG
The AU Core FHIR IG was developed to address the unique challenges of Australia’s healthcare system. It is a localized version of the FHIR standard, designed to ensure consistency and compatibility across a diverse range of healthcare settings. Key aspects include:
- Harmonization with Australian Standards: Aligning FHIR profiles with national standards such as the National Health Information Standards and the Australian Medicines Terminology.
- Focus on Core Data Elements: Defining the structure and usage of essential data elements, including patient demographics, clinical observations, and medication details.
- Regulatory Compliance: Ensuring alignment with the Australian Privacy Principles and other legislative requirements.
Key Features of the AU Core FHIR IG
- Standardized Profiles: The guide defines reusable data profiles for common healthcare scenarios, such as patient identification and diagnostic reporting.
- Terminology Support: Integration with Australian terminologies like SNOMED CT-AU and the Australian Medicines Terminology.
- Interoperability Frameworks: Guidelines for connecting diverse systems, including hospitals, primary care providers, and community health services.
Implications for Australian Healthcare Organizations
The AU Core FHIR IG simplifies the implementation of FHIR by providing a clear roadmap tailored to Australia’s context. Key benefits include:
- Enhanced Data Consistency: Ensuring that healthcare providers exchange data in a standardized format reduces errors and improves care quality.
- Regulatory Alignment: Organizations adopting the AU Core FHIR IG can be confident in meeting legal and compliance obligations.
- Accelerated Adoption: By eliminating ambiguity, the guide reduces the time and resources required to deploy FHIR-based solutions.
Compliance and Integration Pathways
Organizations can leverage the AU Core FHIR IG to streamline their journey toward interoperability. Steps include:
- Assessing Current Systems: Identifying gaps in existing infrastructure and determining the scope of required updates.
- Implementing AU Core Profiles: Configuring systems to comply with the AU Core FHIR IG’s data structures and terminologies.
- Continuous Testing and Validation: Using tools like FHIR validators to ensure ongoing compliance.
The AU Core FHIR IG is a critical enabler of interoperability in Australia, but achieving its full potential requires healthcare organizations to invest in technology readiness, as discussed in the next section.
4. The Need for Healthcare Organizations to Be Technology-Ready
As the adoption of FHIR accelerates, healthcare organizations must ensure they are technologically equipped to implement and leverage this standard effectively. The transition to FHIR is more than a technical upgrade—it is a strategic shift that requires thoughtful planning and investment.
Challenges Faced by Healthcare Providers
- Legacy Systems: Many healthcare organizations rely on outdated systems that are not built for interoperability. These systems require significant modernization to support FHIR.
- Resource Constraints: Limited budgets and workforce capacity can hinder the adoption of new technologies.
- Data Silos: Fragmented data storage across multiple platforms makes integration complex.
Benefits of FHIR Adoption for Healthcare Organizations
Despite the challenges, the rewards of adopting FHIR are substantial:
- Improved Care Coordination: Seamless data exchange ensures that providers have a complete view of a patient’s medical history, leading to better decision-making.
- Operational Efficiency: Automation and standardization reduce administrative workloads and errors.
- Enhanced Patient Engagement: Patients gain secure access to their data, empowering them to participate actively in their care.
Steps to Prepare for FHIR Readiness
- Infrastructure Upgrades: Transition from legacy systems to modern, cloud-based platforms. Invest in scalable and secure data storage solutions.
- Staff Training: Educate clinical and IT teams on FHIR concepts and implementation best practices. Provide hands-on training with FHIR tools and applications.
- Policy Adjustments: Develop internal guidelines for data sharing and security that align with FHIR standards. Establish partnerships with vendors and service providers who specialize in FHIR solutions.
- Piloting and Testing: Start with small-scale pilots to test FHIR integration and resolve challenges before scaling up. Use AU Core FHIR IG as a benchmark for compliance and performance.
Organizations that take proactive steps to become FHIR-ready will be well-positioned to reap the benefits of interoperability, enhancing both their operational capabilities and the quality of care they deliver.
The technological solutions provided by platforms like Microsoft’s Azure Health Data Services FHIR Service make this transition more achievable. Let’s explore these solutions in the next section.
5. Azure Health Data Services FHIR Service: Features and Benefits
Microsoft’s Azure Health Data Services (AHDS) is a game-changer for organizations looking to adopt FHIR. Designed with interoperability, scalability, and security in mind, AHDS simplifies the implementation of FHIR while providing a robust foundation for healthcare data management.
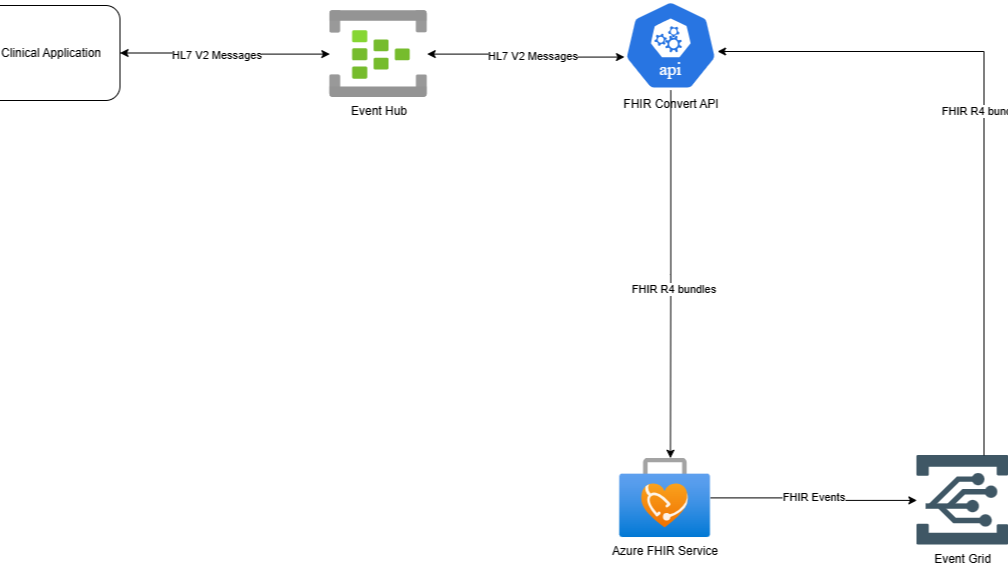
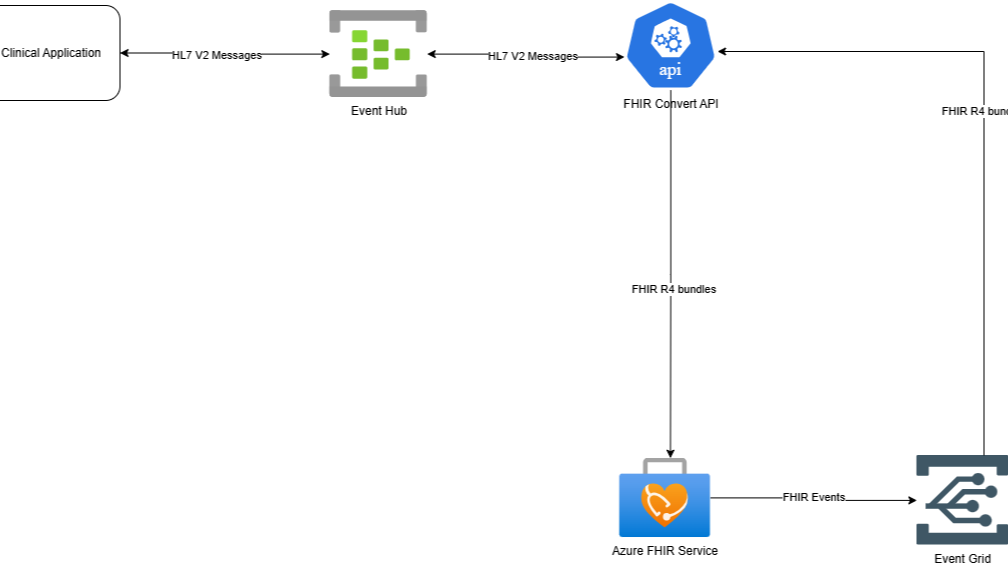
Introduction to Azure Health Data Services
Azure Health Data Services is a fully managed, cloud-based platform that supports healthcare data storage and exchange using FHIR, HL7 v2, and DICOM standards. The platform empowers healthcare organizations to build and deploy interoperable applications quickly and efficiently.
Key Features of AHDS FHIR Service
- FHIR Data Integration: Supports FHIR APIs for seamless data exchange between systems. Enables storage and retrieval of structured healthcare data in FHIR format.
- Advanced Security: Offers built-in security features such as encryption, role-based access control, and compliance with global healthcare standards. Ensures data protection through integration with Azure’s security tools.
- Scalability: Handles large volumes of data with high performance, making it suitable for organizations of all sizes. Supports real-time data processing for critical healthcare applications.
- Analytics and AI Integration: Facilitates advanced analytics using Azure’s AI and machine learning tools. Enables predictive insights for improved decision-making.
Benefits for Healthcare Providers
- Accelerated Interoperability: Organizations can achieve FHIR compliance without building infrastructure from scratch.
- Cost Efficiency: The managed service model reduces the cost and complexity of system maintenance.
- Improved Patient Outcomes: Faster and more accurate data exchange leads to better clinical decisions and patient care.
The Azure Health Data Services FHIR Service provides a strong foundation, but healthcare organizations often require specialized guidance to implement and optimize these solutions. This is where Blue Owls Solutions’ managed service comes in, as detailed in the next section.
6. The Blue Owls Solutions’ Managed Service Around AHDS FHIR Service
Healthcare organizations often face significant challenges when adopting advanced technologies like Azure Health Data Services (AHDS) FHIR Service. Navigating the technical complexities of integration, ensuring compliance, and maintaining operational efficiency require expertise and resources. This is where Blue Owls Solutions steps in with its managed services, designed to simplify and accelerate the journey toward interoperability.
Overview of Blue Owls Solutions
Blue Owls Solutions is a leading provider of technology consulting and managed services, specializing in healthcare data solutions. With a focus on helping organizations harness the full potential of FHIR and AHDS, Blue Owls Solutions offers end-to-end support, from strategy development to system maintenance.
Key Offerings
- Consultation and Strategy Development: Assessment of the organization’s current systems and readiness for FHIR adoption. Development of a tailored roadmap for implementing AHDS FHIR Service.
- Implementation Services: Seamless integration of Azure Health Data Services with existing systems. Customization of FHIR APIs to meet specific organizational requirements. Data migration support, ensuring that legacy data is securely and accurately transferred into the FHIR-based system.
- Compliance and Security: Guidance on meeting regulatory standards, including the Australian Privacy Principles and AU Core FHIR IG. Implementation of advanced security measures, including role-based access controls and encryption protocols.
- Training and Capacity Building: Comprehensive training programs for clinical and IT teams to ensure smooth adoption and operation of the new system. Ongoing support to address challenges and optimize performance.
- Managed Services for Maintenance and Support: Proactive system monitoring to ensure optimal performance and uptime. Regular updates to stay compliant with evolving standards and regulations. Dedicated support for troubleshooting and resolving technical issues.
Benefits of Blue Owls Solutions’ Managed Services
- Reduced Complexity: Blue Owls Solutions handles the technical details, allowing healthcare providers to focus on patient care.
- Cost-Effective: By leveraging managed services, organizations avoid the need for in-house expertise and reduce operational costs.
- Scalability: As healthcare organizations grow, Blue Owls Solutions ensures that systems scale seamlessly to meet new demands.
- Faster Implementation: Expertise in AHDS FHIR Service enables quicker deployment and realization of benefits.
- Enhanced Compliance: By staying up to date with regulatory requirements, Blue Owls Solutions minimizes risks associated with non-compliance.
By leveraging Blue Owls Solutions’ expertise, healthcare organizations can confidently navigate the complexities of FHIR adoption, unlocking the full potential of Azure Health Data Services.
7. Call to Action (CTA): Embrace the Future of Healthcare Interoperability
As Australia’s healthcare sector embraces the vision of interoperability, the adoption of FHIR stands as a critical step forward. From the release of the AU Core FHIR Implementation Guide to advanced solutions like Azure Health Data Services and expert support from Blue Owls Solutions, the tools and resources are available to transform healthcare delivery.
Why Act Now?
- Stay Ahead of the Curve: The move toward interoperability is inevitable. Early adopters will gain a competitive advantage by improving care delivery and operational efficiency.
- Meet Regulatory Standards: With increasing emphasis on compliance, adopting FHIR now ensures readiness for future mandates.
- Enhance Patient Outcomes: Interoperability powered by FHIR translates directly into better, faster, and safer care for patients.
Next Steps
- Explore Your Readiness: Assess your current systems and identify gaps in technology and processes.
- Engage Experts: Partner with Blue Owls Solutions to develop a roadmap tailored to your organization’s needs.
- Leverage Advanced Tools: Harness the power of Azure Health Data Services to streamline data management and exchange.
- Invest in Training and Support: Build capacity within your organization to ensure a successful transition to FHIR.
The adoption of FHIR is reshaping the future of healthcare in Australia. By embracing standards like the AU Core FHIR IG and leveraging cutting-edge platforms like Azure Health Data Services, healthcare organizations can unlock new levels of efficiency, compliance, and patient satisfaction. With the guidance and support of Blue Owls Solutions, the path to interoperability becomes not only manageable but also rewarding.
Don’t wait—start your journey toward a connected healthcare future today.
Contact Blue Owls Solutions Today
Transform your organization’s approach to healthcare data. With Blue Owls Solutions as your partner, you can achieve seamless FHIR adoption, improve patient care, and future-proof your operations.